
Summary
- Barriers Impacting Access: Health and social care professionals face various obstacles, including physical, economic, and cultural barriers that hinder access to services and affect care quality.
- Physical and Economic Challenges: Geographic isolation, high healthcare costs, and inadequate infrastructure contribute to difficulties in accessing necessary treatment, particularly for those in rural areas.
- Cultural and Systemic Issues: Language barriers and cultural beliefs can prevent effective communication and care. Bureaucratic complexities often frustrate both patients and providers, leading to fragmented services.
- Strategies for Improvement: Enhancing accessibility through better infrastructure, improving affordability with financial assistance, promoting cultural competence, and streamlining systems are essential steps to create a more equitable health and social care environment.
Health and social care encompass a broad network of services designed to support individuals’ health and well-being. Although the system strives for accessibility and quality, various barriers pose challenges to achieving these goals. Understanding these barriers, along with their implications, is essential for creating a more inclusive and efficient healthcare environment. This exploration looks into the myriad of barriers in health and social care, providing a detailed analysis.
Barriers in health and social care can be defined as obstacles that prevent individuals from accessing or receiving effective healthcare and support. These barriers can arise from physical, economic, social, cultural, systemic, psychological, and technological factors. Identifying and addressing these barriers is essential for providing equitable and effective care.
Physical Barriers

Geographic Location
Living in rural or remote areas presents distinct challenges. The distance from healthcare facilities can actually impact access to care. This includes:
- Limited healthcare facilities: Sparse distribution in rural areas means people often travel long distances, sometimes without public transport.
- Travel-related issues: Bad weather or poor road conditions can further restrict access, especially in emergency situations.
These geographic barriers can lead to delays in receiving care, potentially worsening health outcomes.
Infrastructure Challenges
Accessibility within healthcare facilities is another essential issue. Poor infrastructure can deter individuals from seeking care. Key concerns include:
- Mobility barriers: Insufficient ramps or elevators can hinder individuals with disabilities.
- Navigation difficulties: Complex layouts and inadequate signage can make it difficult for patients to find their way.
- Facility limitations: Lack of adaptable equipment for those with physical disabilities can limit service provision.
These barriers can create a physical disconnection between patients and the services they need.
Economic Barriers

Cost of Care
Despite the efforts of the NHS, financial constraints continue to affect access to certain services. Patients may face:
- Out-of-pocket expenses: Costs for prescriptions, dental care, or specialised services may not be fully covered.
- Supplementary costs: Travel, childcare, or time off work add additional financial burdens.
Economic barriers can restrict access to necessary care, leading to delayed or forgone treatments.
Insurance and Funding
The complexity of insurance and funding systems can be daunting. Navigating these systems involves:
- Understanding entitlements: Eligibility criteria for benefits and subsidies can be complex and varied.
- Administrative burdens: Lengthy application processes can deter individuals from applying for necessary assistance.
This complexity often results in eligible individuals not accessing the support they need.
Social and Cultural Barriers
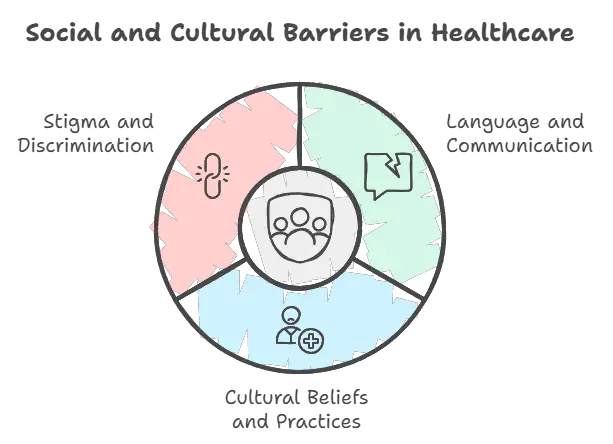
Language and Communication
Clear communication is essential in healthcare settings. Language barriers can result in:
- Misunderstandings: Non-native speakers may struggle with medical jargon, leading to confusion about diagnoses or treatment plans.
- Lack of interpreters: Without access to public interpreters, communication gaps widen, especially during essential interactions.
Cultural Beliefs and Practices
Cultural factors influence perceptions of health and willingness to seek care. Several aspects play a role:
- Traditional healing practices: Some communities may prefer alternative medicine, complementing or replacing conventional care.
- Cultural sensitivities: Practices such as gender-specific care needs can affect comfort in accessing services.
Cultural barriers may lead to reluctance in utilising available healthcare resources.
Stigma and Discrimination
Discrimination and stigma related to race, gender, sexual orientation, or disability affect the healthcare experience:
- Bias from providers: Unconscious bias can lead to differential treatment, impacting the quality of care.
- Self-stigma: Fear of judgment can discourage individuals from seeking help for sensitive issues, like mental health or sexual health concerns.
Removing stigma is an important step towards fostering an empathetic and inclusive healthcare environment.
Systemic Barriers

Bureaucracy and Red Tape
Administrative complexity creates barriers for both patients and providers:
- Appointment hurdles: Long wait times and complicated booking processes delay access to care.
- Documentation requirements: Cumbersome paperwork can overwhelm patients, particularly those with cognitive or literacy difficulties.
Streamlining processes is essential to improve accessibility and efficiency.
Fragmentation of Services
A lack of integration between health and social care services leads to disjointed care:
- Siloed services: Fragmented care provision hinders comprehensive treatment approaches, impacting patient outcomes.
- Inadequate information sharing: Lack of communication between different providers results in incomplete or duplicated service provision.
Integrated care models are essential for providing coordinated and holistic healthcare.
Workforce Challenges
Workforce instability poses significant barriers:
- Staff shortages: Leads to overworked staff with less time for patient engagement.
- High turnover rates: Result in inconsistency in care and lack of continuity for patients.
Addressing workforce challenges enhances both the quality and availability of care.
Psychological Barriers
Fear and Anxiety
Fear can inhibit individuals from engaging with healthcare services:
- Fear of diagnosis: Concerns about being diagnosed with a serious condition may prevent people from seeking medical attention.
- Anxiety around procedures: Embarrassment or fear of medical environments can lead to avoidance of necessary treatments.
Providing supportive environments can help alleviate fears and encourage engagement.
Lack of Trust
Trust is foundational to the patient-provider relationship:
- Historical mistreatment: Past negative experiences can foster mistrust in the system.
- Perceived insensitivity: Lack of compassion or understanding from healthcare providers can erode trust.
Building trust requires transparent communication and empathetic care.
Technological Barriers

Digital Divide
The disparity in access to digital resources affects healthcare accessibility:
- Lack of technology: Some individuals lack access to internet or digital devices, essential for telehealth services.
- Digital literacy: Older adults or those less familiar with technology may struggle with using online platforms.
Addressing the digital divide ensures that technological advancements benefit all individuals.
Data Privacy Concerns
Confidence in data security is paramount:
- Privacy fears: Concerns about how personal health data is stored and shared can deter usage of digital health services.
- Security breaches: Anxiety over potential data breaches may prevent people from engaging fully with digital health innovations.
Implementing robust security measures is essential for fostering trust in digital health platforms.
Ways to Overcome Barriers
Addressing barriers in health and social care necessitates a comprehensive and integrated approach. Below are some key strategies:
Enhancing Accessibility
- Infrastructure improvements: Invest in facilities to ensure they cater to all abilities, with accessible entrances and amenities.
- Outreach programmes: Develop mobile health clinics to reach underserved communities, bridging geographical gaps.
Improving Affordability
- Subsidies and financial aid: Enhance support for out-of-pocket expenses, ensuring treatments are financially accessible.
- Simplified funding: Streamline funding processes, making applications more straightforward and eligibility clearer.
Promoting Inclusivity
- Multicultural training: Provide staff with cultural competence training to better understand and meet diverse needs.
- Enhanced language support: Offer interpreters and translated materials, ensuring clear communication for non-native speakers.
Streamlining Systems
- Administrative digitalisation: Implement digital solutions to simplify appointment scheduling and reduce paperwork.
- Integrated systems: Promote collaboration between different care providers to ensure seamless patient journeys.
Enhancing Workforce Stability
- Incentives for retention: Improve working conditions and offer professional development opportunities to retain skilled staff.
- Supportive environments: Foster a positive workplace culture to reduce burnout and enhance job satisfaction.
Building Trust and Engagement
- Patient involvement: Engage patients in decision-making, ensuring their voices are heard and respected.
- Feedback mechanisms: Implement regular feedback loops to identify areas for improvement and build trust within the community.
Final Thoughts
The barriers in health and social care are complex and multifaceted. Overcoming them requires collaboration across government, healthcare providers, and communities. Efforts must focus on enhancing accessibility, affordability, inclusivity, and trust. By systematically addressing these barriers, the UK’s health and social care system can become more responsive, equitable, and effective. Continuous adaptation and community engagement are essential to ensure all individuals receive the quality care they deserve, creating a healthier nation for all.
Glossary and Key Terms
- Accessibility
The ease with which people can reach and use healthcare services. It includes physical access to facilities and the availability of services. - Bureaucracy
The complex administrative processes that can slow down access to care. It often involves many forms and approvals. - Cultural Competence
The ability of healthcare providers to understand and respect diverse cultural backgrounds. This helps in providing better care to all patients. - Discrimination
Unfair treatment of individuals based on characteristics like race, gender, or disability. It can lead to reluctance in seeking care. - Economic Barriers
Financial obstacles that prevent individuals from accessing healthcare. This includes high costs for treatments and medications. - Fragmentation of Services
When health and social care services do not work together effectively. This can result in disjointed care for patients. - Integrated Care Models
Approaches that encourage collaboration between different healthcare providers. This aims to provide a more cohesive experience for patients. - Language Services
Support offered to help patients communicate effectively with healthcare providers. This includes interpreters and translated materials. - Psychological Barriers
Emotional factors that hinder people from seeking care. Fear and anxiety about healthcare experiences can play a significant role. - Stigma
Negative perceptions associated with certain health conditions. Stigma can prevent individuals from seeking necessary help or treatment.
Subscribe to Newsletter
Get the latest news and updates from Care Learning and be first to know about our free courses when they launch.






