
This guide will help you answer 1.2 Explain what is meant by the mental health continuum.
The idea of the mental health continuum is a helpful way to understand mental health. It shows that mental health is not just about having a mental illness or being healthy. Instead, it sees mental health as a range or a scale.
What Is the Mental Health Continuum?
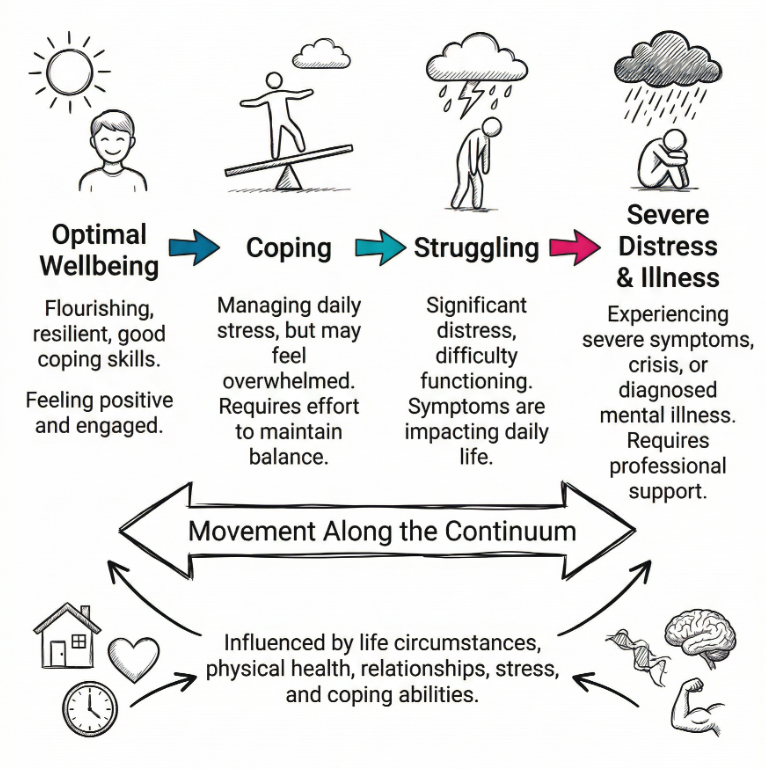
The mental health continuum is a way of thinking about mental health as being on a scale or spectrum rather than simply being in one of two fixed states, such as “healthy” or “unwell”. It suggests that mental health exists across a range, from optimal wellbeing at one end through to severe mental distress and illness at the other. People can move back and forth along this continuum throughout their lives, depending on a number of internal and external factors.
This approach recognises that mental health is not static. It changes over time and can be affected by life circumstances, physical health, relationships, stress, and coping abilities. Everyone has mental health, just as everyone has physical health. It is not only relevant for those diagnosed with a mental illness. Instead, it applies to all individuals, regardless of their current state of wellbeing.
The Scale of Mental Health
When describing the mental health continuum, it helps to think of it as having several points along a scale. At one end are people who are in good mental health. They experience positive moods, have high levels of functioning, and are able to enjoy daily activities. They may still encounter stress or challenges but have effective coping mechanisms.
In the middle of the continuum, people might be experiencing some mental health difficulties such as mild anxiety, sleep disruption, or feelings of low mood. These issues may be temporary and might not require medical intervention but can still interfere with day-to-day life.
At the far end are those who have significant mental health problems or diagnosis such as severe depression, psychosis, bipolar disorder, or other conditions that greatly reduce their ability to function without professional help.
Movement Along the Continuum
Mental health does not remain fixed for anyone throughout life. A person can shift towards positive wellbeing or towards distress depending on situations and experiences. Positive changes might include improving lifestyle habits such as nutrition, physical activity, and maintaining social connections. Negative changes can occur through prolonged stress, trauma, loss, or physical illness.
These movements can be temporary or long term. For example, someone might experience high stress during examinations which places them nearer to the distressed end of the continuum. After the examinations, with relaxation and rest, they may move back towards wellbeing.
Factors Affecting Position on the Continuum
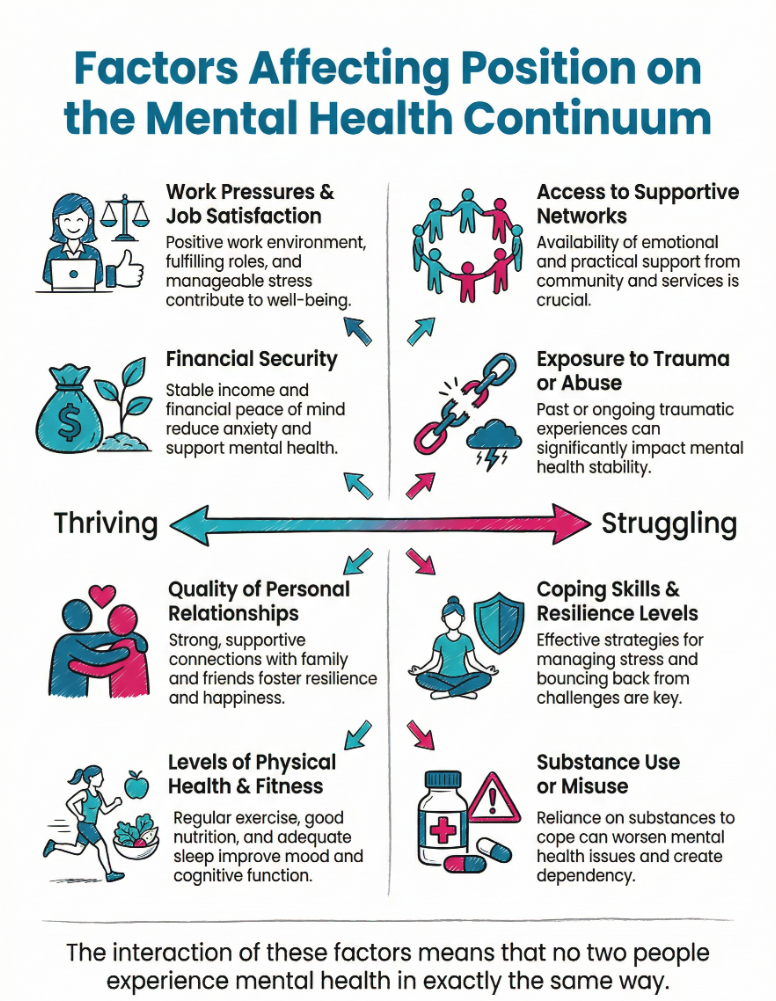
Multiple factors can push individuals in either direction along the mental health continuum. They include:
- Work pressures and job satisfaction
- Financial security or insecurity
- Quality of personal relationships
- Levels of physical health and fitness
- Access to supportive networks
- Exposure to trauma or abuse
- Coping skills and resilience levels
- Substance use or misuse
The interaction of these factors means that no two people experience mental health in exactly the same way.
Preventive and Protective Measures
People can take measures to help maintain or improve their position on the mental health continuum. This involves both personal actions and support from others. Strategies include:
- Regular exercise to support mood regulation
- Healthy sleep routines
- Maintaining balanced nutrition
- Practising stress management techniques such as mindfulness
- Talking openly with trusted friends or family about feelings
- Seeking professional help early before problems become severe
These measures do not guarantee perfect mental health, but they can help reduce the risk of moving towards the distress end of the continuum.
The Role of Self-Awareness
Self-awareness plays an important role in recognising where a person might currently sit on the continuum. By noticing signs such as increased irritability, loss of interest in pleasurable activities, or constant tiredness, individuals may be able to identify early shifts towards distress. Early recognition can allow action to be taken to prevent escalation.
Some people use mood journals or regular check-ins with friends to monitor changes. Others rely on professional assessments from counsellors or doctors.
Impact on Daily Life
Position on the mental health continuum affects many areas of daily life. At the wellbeing end, individuals are likely to manage stress well, meet commitments, think clearly, and have strong relationships. Closer to the distress end, people may find decision making difficult, withdraw from social contact, or struggle to maintain responsibilities such as employment or childcare.
Understanding the continuum helps employers, educators, and communities offer the right level of support at the right time. It encourages a focus on maintaining wellbeing rather than only reacting once serious illness develops.
Stigma Reduction
One benefit of viewing mental health as a continuum is that it can reduce stigma. This perspective normalises that anyone can experience poor mental health at different times, just as anyone can experience physical health problems. It shifts thinking away from “us” and “them” and towards the idea that mental health changes for everyone.
With less stigma, people may be more willing to seek help early, which can prevent worsening conditions.
Professional Use of the Continuum
Mental health professionals often use the concept of the continuum to assess individuals and to plan interventions. By identifying where someone currently sits and the factors influencing them, they can tailor their support to encourage a shift towards wellbeing.
This approach works not only for those diagnosed with illnesses but for anyone experiencing difficulties in coping. It is used in schools, workplaces, and communities as part of wellbeing programmes.
Final Thoughts
The mental health continuum is a way of viewing mental health as a shifting state rather than a fixed condition. It spans from optimal wellbeing to severe distress and includes all points in between. Everyone moves along the continuum throughout life, influenced by personal and environmental factors.
By recognising mental health as fluid, people and communities can take proactive steps to maintain wellbeing, respond early to signs of trouble, and create supportive environments. This model encourages understanding, reduces stigma, and promotes the idea that mental health is a shared human experience.
Subscribe to Newsletter
Get the latest news and updates from Care Learning and be first to know about our free courses when they launch.





